can change the world.

can change the world.

can change the world.
can change the world.


can change the world.

can change the world.

can change the world.
Welcome To
The Smile Architects
We believe smiles can change the worldThe Smile Architects experience is a personal journey for you and your family. Our top-caliber team is dedicated to supporting, serving, and solving every patient's needs through a unique dental experience, customized service, and relationship driven visits. We are experts in the field, take great pride in our craft, and are committed to doing the best quality of work. We create smiles that stand the test of time and have the potential to change our patient's lives. A smile is the door to the heart of your being. Once opened, it profoundly expresses who you are. We believe smiles can change the world. And for us, it starts with yours.
THE SMILE ARCHITECTS
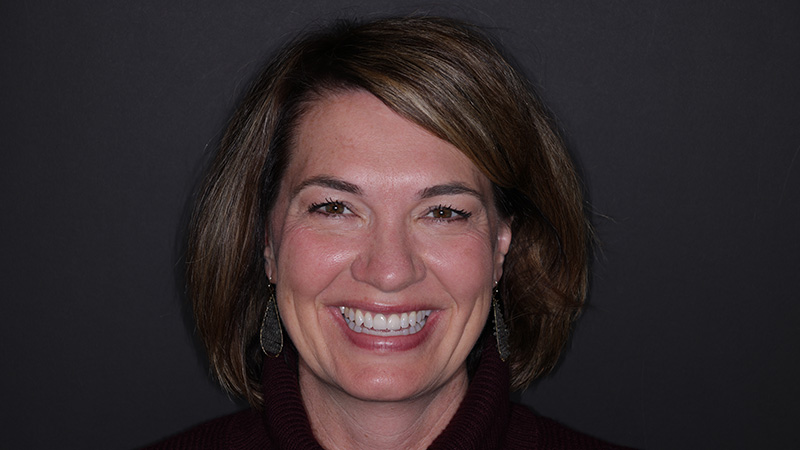
Meet Your Dental Family
"Our entire team prides itself on providing the most warm, caring and friendly experiences for all of our patients." - Dr. Cooper















THE SMILE ARCHITECTS
Our Dental Services
We are a full service Dental Practice that executes top quality care no matter your personal needs or goals.THE SMILE ARCHITECTS
No guest too small
It’s never too early to start good habits. We pride ourselves on providing expert quality dentistry for your entire family.


THE SMILE ARCHITECTS
Meet the team
We pride ourselves on having a team of top-caliber dentists, clinical staff and front office team. We use our expertise, skills and warmth to ensure you get a tailor made dental journey.
WELCOMING NEW PATIENTS
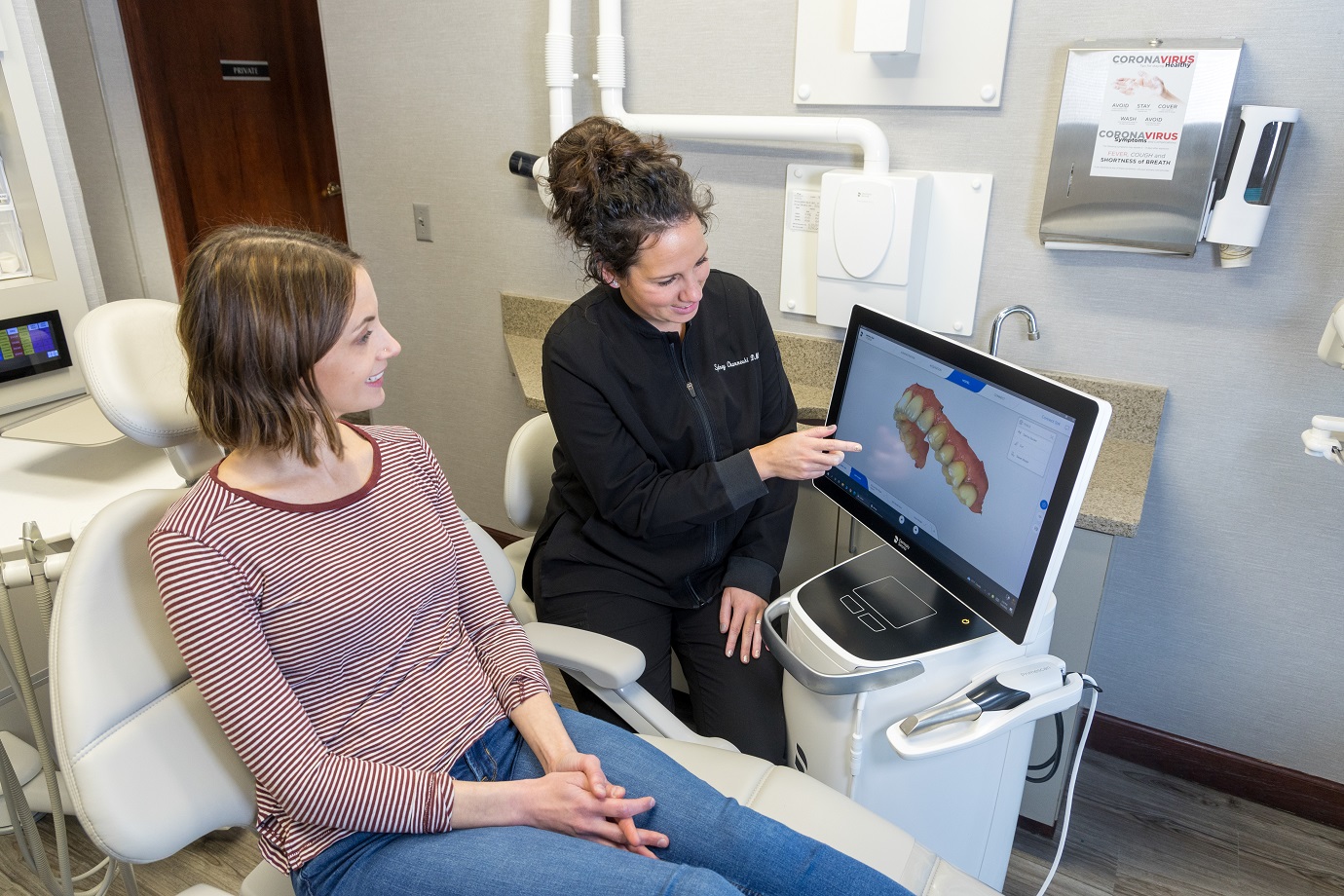
Providing you with a top caliber dental experience
All your appointments will take place in our state of the art office environment with comfortable rooms and individualized care.
Our Patients say
“Great dental facility and the staff is wonderful. Always leave there feeling they were completely honest and straightforward with me about my health. I've been seeing Dr. Cole for at least 15 years, she has my full trust and I have zero interest in finding another dentist.”Nicholas, Google Review
Our Patients say
“They are so accommodating to all your needs. They make you feel so comfortable. I always hated going for dental appointments, but not so much anymore!”Matt, Google Review
Our Patients say
“Dr. Cooper and the entire Roscher Group are just fantastic. The atmosphere is very friendly and welcoming and the staff are caring and professional. Not to mention my dental care is top notch and my smile is beaming with confidence.”Brenda, Facebook Review
Our Patients say
“Wonderful dental practice, warm and inviting. The front desk staff is always welcoming and easy to work with on scheduling and billing, the hygienists are so nice and do great work, and Dr. Cooper and Dr. Cole are amazing…”Kate, Facebook Review
Ready To Improve Your Smile?
Virtual Smile Consultations With The Smile Architects
The Smile Architects is offering Virtual Smile Consultations. Simply follow the instructions below to begin.
UPLOAD
Upload a selfie style photo of your smile.
OUR TEAM
Our Team will put together recommendations and send via email.
SCHEDULE
We’ll then schedule a VideoChat or in-office visit to explore your options.

Get in Touch
We’d love to join you on your dental journey.
We’re here to help: 651-459-2387